
Depicted in this watercoloured etching, The Ancient of Days, by William Blake,
is Urizen, a figure that for Blake embodied reason and law.
Urizen’s outstretched hand holds a compass over the darker void below,
representing an event in the Book of Proverbs,
‘when he set a compass upon the face of the earth’
(image via the British Museum).
This is the first in a series of articles being published by the International Livestock Research Institute (ILRI) in the lead up to the High-Level Meeting on Antimicrobial Resistance, which will be held in the margins of the 71st session of the United Nations General Assembly, attended by heads of state and government at the UN’s New York City headquarters on 21 Sep 2016. Global leaders at the summit will commit to leading the fight against antimicrobial resistance, including the all-important resistance to antibiotics. Following statements from the World Health Organisation (WHO), the Food and Agriculture Organisation (FAO) and the World Organisation for Animal Health (OIE), a declaration emphasizing the five strategic objectives of the World Health Assembly’s Global Action Plan on Antimicrobial Resistance will be submitted for adoption by the UN General Assembly.
Scientists from the International Livestock Research Institute (ILRI) and partner organizations this week published a must-read article on the ‘One Health’ as well as ‘One World’ aspects of the rapid rise of antimicrobial resistance (AMR) in pathogenic organisms.
The UN declaration on antimicrobial resistance, says ILRI’s Tim Robinson, lead author of the new scientific article, ‘should place national governments under pressure to take action towards reducing consumption of antibiotics in both human medicine and agriculture.’
Apocalyptic AMR numbers
In May this year, the long-awaited final report from the Review on Antimicrobial Resistance, which was commissioned by the UK Government and Wellcome Trust, was published. The report, Tackling drug-resistant infections globally, recommends four main actions: (1) conducting a global public awareness campaign, rewarding developers of (2) new antibiotics and (3) rapid diagnostic tests for microbial infections and (4) reducing overuse of antibiotics in agriculture.
The report presents some apocalyptic figures but the truth is that we really don’t know what the burden is, how it is likely to change or what contribution to that is made by antibiotic use by the livestock sector.
—Tim Robinson
But, Robinson adds, ‘The problem is already immense and is growing rapidly. We have been squandering our antibiotic resources for far too long and immediate action is needed on a very large scale if we are to reverse current trends.’
What follows are excerpts from the paper by Robinson and his colleagues, Antibiotic resistance is the quintessential One Health issue, published in the Transactions of the Royal Society of Tropical Medicine & Hygiene on 29 Jul 2016.
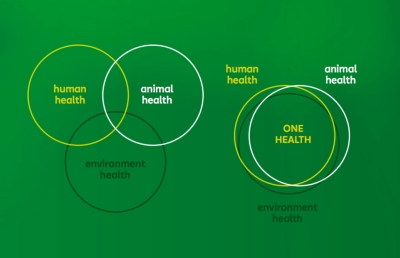
One Health diagram from the One Health Platform (onehealthplatform.com)
AMR is a ‘One Health’ (people-animals-environment) issue
It is difficult to imagine an issue that epitomises the principles of One Health more than AMR does. The One Health approach . . . recognises that the health of people is connected to the health of animals and the environment.
—Tim Robinson
Human health: Of the three domains, human health takes the spotlight, with multidrug-resistance genes now highly prevalent in many important and common pathogens like Escherichia coli, Klebsiella pneumoniae and Staphylococcus aureus. Quite apart from the many infectious diseases for which we rely on antibiotics to combat, these drugs underpin modern medicine by allowing us to carry out common surgical procedures and treatments that depress the immune system, such as chemotherapy to treat cancer. . . .
Animal health: [T]he published estimates of the proportion of antibiotics consumed in animal agriculture—84% (for 36 antibiotics) in China and 70% in USA—suggest global agricultural consumption probably exceeds that of humans. A large part of this use is justified and valid on veterinary grounds, but there is much misuse in the agricultural sector. With such large consumption levels it seems likely that agricultural use contributes significantly to AMR. . . .
Environmental health: . . . Environmental bacteria, being quantitatively the most prevalent organisms, serve as sources for AMR genes that can become incorporated, over time, into pathogens of people and animals.
AMR is also a One World issue
‘As well as being a One Health issue, AMR is a One World issue. The globalisation of the food system, with increasing movement of livestock and agricultural produce, combined with increasing human travel, facilitates the rapid spread and mixing of AMR genes that emerge. . . .
Like . . . carbon emissions, no matter how good a country’s programme of antimicrobial stewardship in health and agriculture, they are laid bare to the importation of AMR genes that have emerged and spread from other parts of the world.
—Tim Robinson
‘. . . The other factor making AMR a One World issue is that dealing with AMR is central to the long-term economic development of countries and to our global well-being. LMICs [low-to middle-income countries] face the greatest burden of AMR because of their disease-prone environments, poorer sanitary standards and, for the poorest, much reduced access to effective antibiotics. Poor access to competent veterinary and extension services leaves farmers in LMICs with antibiotics as their only resource to tackle endemic bacterial animal infections. Interventions must be based on an understanding of and respect for the different social and socio-economic contexts in which they are to be implemented.
AMR is a global problem calling for global solutions: but the solutions will not be the same in every country, or among different socio-economic groups.
Some use antimicrobials too much, some too little and many use them unwisely: understanding patterns of use and incentives for changing these, and exploring alternative options, must underpin any reduction efforts.
‘. . . [AMR] is not a problem that HICs [high-income countries] will be able to solve alone. The important role that animal agriculture plays in livelihoods in LMICs is unknown or underestimated by many in HICs and needs to be an integral part of the thinking and negotiation if we want to avoid the pitfalls seen in climate negotiations, with LMICs often reluctant to take measures that may compromise their short-term economic development. . . .’
Integrated approaches to reduce selection pressure and disrupt AMR transmission cycles on a global scale must be sought that are founded not only on sound One Health principles, but also based on economic evidence and on principles of social equity and global access to effective healthcare for people and their animals.
Acknowledgments
This work was made possible through a Wellcome Trust Our Planet, Our Health planning grant [201848/Z/16/Z] and was further supported by CGIAR Fund Donors under the CGIAR Research Program on Agriculture for Nutrition and Health.
Read the whole scientific paper
Antibiotic resistance is the quintessential One Health issue in the Transactions of the Royal Society of Tropical Medicine & Hygiene, 29 Jul 2016, written by the following:
Timothy Robinson (ILRI)
Dengpan Bu (Chinese Academy of Agricultural Sciences)
Juan Carrique-Mas (Oxford University Clinical Research Unit in Vietnam)
Eric Fèvre (University of Liverpool and ILRI)
Marius Gilbert (Université Libre de Bruxelles)
Delia Grace (ILRI)
Simon Hay (University of Washington, USA, and Oxford Big Data Institute at the Li Ka Shing Centre for Health Information and Discovery of Oxford University)
Jatesada Jiwakanon (Khon Kaen University, Thailand)
Manish Kakkar (Public Health Foundation of India)
Sam Kariuki (Kenya Medical Research Institute)
Ramanan Laxminarayan (Center for Disease Dynamics, Economics and Policy, USA)
Juan Lubroth (Food and Agriculture Organization of the United Nations)
Ulf Magnusson (Swedish University of Agricultural Sciences)
Pham Thi Ngoc (National Institute of Veterinary Research, Vietnam)
Thomas Van Boeckel (Swiss Federal Institute of Technology)
Mark Woolhouse (University of Edinburgh)
READ MORE
The 21 Sep 2016 UN High-Level Meeting on Antimicrobial Resistance
UN High-Level Meeting on Antimicrobials—what do we need?, commentary published in The Lancet by Ramanan Laxminarayan, Carlos Amábile-Cuevas, Otto Cars, Timothy Evans, David Heymann, Steven Hoffman, Alison Holmes, Marc Mendelson, Devi Sridhar, Mark Woolhouse and John-Arne Røttingen, 16 Jul 2016. Excerpt:
‘The UN General Assembly High-Level Meeting of Heads of State will discuss sustainable access to effective antimicrobials in September, 2016. The meeting must develop realistic goals, stimulate political will, mobilise resources, and agree on an accountability mechanism for global collective action on this issue. . . . We believe that the UN General Assembly High-Level Meeting should establish a UN High-Level Coordinating Mechanism on Antimicrobial Resistance (HLCM) with four core functions’:
(1) Raise awareness about lack of access to antibiotics and drug resistance
(2) Establish, monitor and report on global and national enforceable targets
(3) Finance implementation of global and national level action plans and a global coordination and monitoring platform
(4) Support member states to pursue national level, multisectoral action for implementation of WHO’s Global Action Plan on Antimicrobial Resistance alongside national efforts to improve access to effective antimicrobials.
United Nations prepares to tackle antibiotic resistance, commentary by Molly Miller-Petrie published on the Center for Disease Dynamics, Economics and Policy (CDDEP) blog, 26 Jul 2016. Excerpts:
‘On June 29 [2016], Ambassador Gómez Camacho, Mexican Permanent Representative to the U.N. and lead for the high-level meeting, invited CDDEP to speak to the U.N. Member States as a part of a civil society panel on antimicrobial resistance. . . . Each organization presented their view on what should be included in the final outcome document, after which member states were able to ask questions of the experts directly. A similar panel was conducted with members of industry the following week. As the only participating organization with a major focus on low- and middle-income countries, CDDEP was also invited to speak to the Group of 77 Member States plus China, representing 134 low- and middle-income member countries. On July 18, CDDEP Director Dr. Ramanan Laxminarayan and Molly Miller-Petrie met with the group at the U.N. Headquarters to address the particular challenges of combatting resistance in low-resource settings. . . .’
Earlier research on antimicrobial use in food animals
Global trends in antimicrobial use in food animals, by Thomas Van Boeckel (Princeton University), Charles Brower (Center for Disease Dynamics, Economics & Policy [CDDEP]), Marius Gilbert (Université Libre de Bruxelles), Bryan Grenfell (Princeton University), Simon Levin (Princeton), Timothy Robinson (ILRI), Aude Teillant (Princeton) and Ramanan Laxminarayan (CDDEP), published in the Proceedings of the National Academy of Science, early edition, 20 Mar 2015. See also a report of this PNAS paper on the ILRI News blog, First global map of the rising use of antimicrobial drugs in farm animals published in PNAS (25 Mar 2016), and also reports published on the ILRI Clippings blog, Reuters: Livestock in poor countries need drugs to stay alive and productive, but how to avoid the rise of ‘super bugs’? (23 Mar 2015) and New publication warns of rising use of antibiotics and other antimicrobial drugs in farm animals (30 Mar 2015).
Animal production and antimicrobial resistance in the clinic, a commentary published in The Lancet, by Timothy Robinson, Heiman Wertheim, Manish Kakkar, Samuel Kariuki, Dengpan Bu and Lance Price, published online 18 Nov 2015, DOI: http://dx.doi.org/10.1016/S0140-6736(15)00730-8. See also a report of this Lancet commentary published on the ILRI News blog, Limiting use of antibiotics in livestock production to stem growing antimicrobial resistance in human pathogens (31 Dec 2015).
Review of evidence on antimicrobial resistance and animal agriculture in developing countries, by ILRI’s Delia Grace, published Jun 2015, DOI: http://dx.doi.org/10.12774/eod_cr.june2015.graced. This 44-page report was produced by ILRI with the assistance of the UK Department for International Development and its ‘Evidence on Demand’ hub. The report identifies key evidence gaps in our knowledge of livestock- and fisheries-linked antimicrobial resistance in the developing world and documents on-going or planned research initiatives on this topic by key stakeholders.
ILRI-Liverpool project tracking microbial flows in Nairobi
Slum farming and superbugs—An ‘Urban Zoo’ science project tracks bacterial routes in complex environments, 29 Dec 2015, a review posted on the ILRI Clippings blog about two news reports: Scientists study slums for signs of spreading superbugs, by Steve Baragona at Voice of America (23 Dec 2015), and Mapping for food safety: How and why communities in Nairobi’s informal settlements are creating and using maps to ensure their food and the people who sell it are safe, by Paolo Cravero on the International Institute for Environment and Development blog (21 Dec 2015).
All things zoonotic: An ‘Urban Zoo’ research project tracks livestock-based pathogen flows in and around Nairobi, 31 Mar 2015, a report published on the ILRI Clippings blog covering, among other publications, a news report about an ILRI-Liverpool project published in the New Scientist, Mapping the web of disease in Nairobi’s invisible city (30 Aug 2014).
Recent ILRI essay on emerging infectious diseases and disease plagues
Pandemic proofing the world: An epidemiologist in Nairobi on the next Zika virus, by ILRI’s Delia Grace, published in How We Get to Next, on Medium (29 Jun 2016), and on the ILRI News blog (26 Jul 2016).